Plantar Fasciitis Treatment
- Eclipse Wellness

- Apr 8, 2022
- 9 min read
Updated: Jul 3, 2023
What Is Plantar Fasciitis?
Plantar fasciitis is a common pathology of the feet that can cause severe pain and disability with running, walking, jumping, and other movements. It is also one of the least understood conditions regarding diagnosis and treatment. I believe that plantar fasciitis is overdiagnosed and poorly treated by a majority of healthcare professionals. To start, let’s look at the anatomy of the bottom of the foot.

This image shows the shallowest of the three commonly accepted layers of muscle in the foot. The plantar aponeurosis is another name for the plantar fascia. Fascia is a thick connective tissue that runs throughout our bodies and provides support to most structures. In some areas such as the bottom of the foot (also the IT band), we have thicker fascia to provide support and reduce stress. The plantar fascia is really strong, like really really strong. So strong that it takes over 1,000 pounds of force to deform it by 1% (this will be important later on).
The image above does not show that the flexor digitorum brevis actually inserts into the calcaneus (heel bone) by itself and is not completely connected to the plantar fascia. The flexor digitorum brevis helps curl your toes. It is important to understand that the plantar fascia is not a muscle. If you dorsiflex your foot as if you are stretching your calf, you will stretch the fascia, and squeezing your toes shortens it. However, it is not contracting in the same way that a muscle would.
Another purpose of the plantar fascia is to maintain your foot arch. We have arches in our feet for force absorption and creation. When you step, your foot pronates and your arch collapses to absorb force. As you progress to step forward, your foot supinates and your arch increases to propel you forward. Part of the impetus to tighten the arch comes from your big toe extending and tightening the plantar fascia. This is known as the windlass mechanism and it is pictured below courtesy of physio-pedia.com

So, the purpose of the plantar fascia is to absorb force in the foot, but also to maintain the arch and help distribute and produce force when walking. This is why it is so strong and resists deformation. Imagine how much force goes through your foot with every step you take, let alone if you are running. It is amazing how strong our bodies are!
Here are the other layers of the foot, starting with the middle layer of muscles:

The lumbricals help you squeeze and separate your toes together. The quadratus plantae is an odd muscle whose entire function is to help another muscle. It pulls the flexor digitorum longus into a more optimal position to flex the toes. The flexor digitorum longus originates from the back of your tibia in your lower leg and runs through the bottom of your foot to your toes. The quadratus plantae helps keep it on an optimal line to flex your toes. Note where the quadratus plantae is located, almost directly under your plantar fascia.
The final and deepest layer of muscles is shown below:

The flexor digiti minimi brevis flexes your little toe and helps maintain the outside arch of your foot. The flexor hallucis brevis flexes your big toe and actually originates from a few bones in your midfoot including your cuboid. The cuboid bone is pictured below:

The bone is in the middle of your foot on the outside. Therefore, the flexor hallucis brevis must travel from the outside of your foot to your first toe on the inside of your foot. This puts the muscle directly under your plantar fascia (hopefully you see where all of this is going).
How to Diagnose Plantar Fasciitis
There are several factors that lead to a diagnosis of plantar fasciitis. The primary sign is sharp, possibly stabbing pain near the heel. This pain is typically worse first thing in the morning because we usually point our toes while sleeping, which tightens the fascia and surrounding tissues. The first few steps provide a stretch on the tissues that have been shortened for several hours, usually resulting in pain. Pain can also be severe after prolonged sitting or if you run or walk for a long distance.
Imaging is not often used for plantar fasciitis as there is not much to see. X-rays can make sure that a stress fracture is not present in one of the bones in your foot. X-rays can also look for bone spurs at the heel. These spurs can occur from tight muscles and the plantar fascia pulling on the calcaneus or heel bone. Your body will lay down more bone to protect against stress, leading to spurs. Interestingly, the American Academy of Orthopaedic Surgeons notes that 10% of all people are shown to have heel spurs, but only 5% of those who have them actually suffer from pain. It is important to understand that just because imaging reveals a heel spur, it is not necessarily the cause of your symptoms.

If you go to a healthcare provider with the symptoms described above, they will probably diagnose you with plantar fasciitis. If they take the time to have you remove your shoe, they will poke you around your heel and probably say “you have plantar fasciitis”. It is important to remember the anatomy that I showed you above. There are multiple muscles that run around and below the plantar fascia. A brief assessment can rule out a strain in those muscles, which should be treated differently than plantar fasciitis.
One of the easiest ways to assess whether the plantar fascia or muscles are causing your symptoms is to flex your toes. The plantar fascia should feel much more pain with stretching of your foot, and squeezing your toes should relieve some of the pain. However, if muscles are involved, this can worsen your symptoms. Stretching the foot can cause pain if there is muscular involvement, because you are stretching the muscles along with the plantar fascia.
A skilled clinician should also be able to palpate the individual muscles. The flexor digitorum brevis will contract if you squeeze your four toes other than your big toe. The flexor hallucis brevis will contract if you only squeeze your big toe. There are other muscles that can be involved, but these are two simple ones to rule out. If you feel along the bottom of your foot while flexing and relaxing your big toe, particularly on the middle and outside of your foot, then you should feel the flexor hallucis brevis. Similarly, if you flex your other four toes, you will feel the flexor digitorum brevis and longus contract. You do not need to necessarily isolate which muscle is the issue if you are self-diagnosing, but it is important to know if it is a muscular problem.
Plantar Fasciitis Treatment
The good news is that conservative care primarily focused on physical therapy improves 90% of people within 10 months according to the American Academy of Orthopaedic Surgeons. 10 months is a long time frame, but these conditions typically take longer to heal than we imagine. Also, our feet are constantly in use, so it is harder to give relative rest and then increase workload. If you hurt your arm, you can use the other one and gradually re-introduce activities to the hurt arm. That is not an option for your foot.
Manual therapy can be beneficial to decrease pain and improve mobility temporarily. It is important to remember that the plantar fascia needs over 1,000 pounds of force to deform 1% so pushing as hard as you can on your foot is probably not changing its configuration. However, targeting the calf and foot muscles can allow for increased mobility in the surrounding tissues, which can help offload the plantar fascia. Trigger point dry needling is an effective way to treat the deep muscles of the foot that are difficult to palpate. The needle allows for targeted release of the affected muscles.

Night splints are often given to people to stretch the plantar fascia and calf overnight so that they are not as tight in the morning. Anecdotally, I have seen some people benefit from night splints, but I have also seen many people get no benefit or have worse sleep. The issue with sleeping may not just be the shortening of the plantar fascia and muscles, but also the fact that there is little movement and blood flow in the area. This is not solved by a splint, as it is just putting the foot in a different position to stiffen. Unfortunately sleep is a necessity, so it is best to give yourself time to gently stretch in the morning before jumping out of bed.
Orthotics can be helpful in certain cases, and I prefer simple over-the-counter ones to custom orthotics unless absolutely necessary. Supporting the foot can allow the injured tissue to heal and heel cups can be beneficial to raise the heel and decrease the stress and tension on the plantar fascia and foot muscles. Walking boots can be used in extreme cases, but these are temporary solutions to decrease pain and allow for exercise progression. It is important to think about the true diagnosis that you may require. If you strained a muscle then a walking boot for 4 weeks may decrease your pain temporarily, but it is not doing anything to strengthen the muscle and prevent long term recurrence of your symptoms.
More aggressive interventions include steroid injections into the plantar fascia to limit swelling. There is a limit to how many injections you can undergo because they can cause breakdown of the fascia. Platelet-rich plasma or PRP is a relatively new process that involves removing the healing factors from your blood and injecting them directly into an injury with the hope of kickstarting your body’s healing process. A systematic review by Hurley, et al. showed that PRP delivered superior outcomes at 6 months and beyond compared to steroid injections. This makes some sense as steroid injections will eventually dissipate into the surrounding tissue. Interestingly, another systematic review by Hohmann, et al. found benefits from PRP compared to steroid injections from 3 months to 1 year after the procedure. However, they noted that the current literature is extremely limited and of poor quality. Also, PRP procedures vary by the medical provider, so benefits in one study do not necessarily predict benefits for others. Biological agents like PRP do offer an interesting alternative to steroid injections, but significant research remains.
If conservative treatment is ineffective, then surgery is a last resort. The most common surgery is to simply cut the plantar fascia to reduce the symptoms. This can be effective, but it is removing an anatomical structure that provides support to your foot.
Plantar Fasciitis Exercises
Exercises for plantar fasciitis are typically not addressing the problem. Rolling your foot on a lacrosse ball may feel good from temporary blood flow and a strong sensation other than pain. However, you are probably not putting 1,000 pounds of force into the ball and therefore you are not mobilizing the fascia. If it feels good to roll your foot on a ball then go right ahead, but it is not fixing your problem. The image below is courtesy of gearjunkie.com

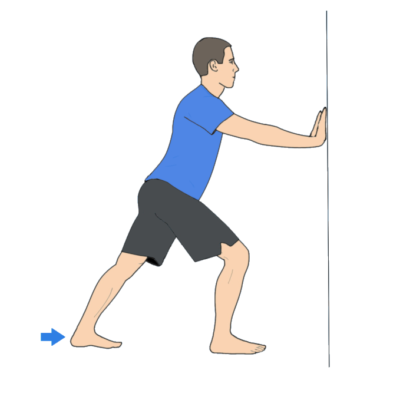
The plantar fascia is a continuation of your calf muscles and achilles tendon. Limited dorsiflexion is a risk factor for plantar fasciitis according to Riddle, et al. Stretching of the calf as shown below can be beneficial in decreasing stress on the plantar fascia. I have talked about this before, but make sure to turn the back foot towards the front foot and keep your weight on the outside of the back foot for an optimal calf stretch. The image below is courtesy of fixflatfeet.com
Similar to calf stretching, mobilizing the talocrural joint can be helpful for increasing dorsiflexion. There are many ways to mobilize the joint, but the simplest is pictured below courtesy of theprehabguys.com

The plantar fascia runs from the heel to the big toe, so limitations in big toe mobility can increase stress onto the fascia. Our big toes should extend 60 degrees for normal walking mechanics. You can mobilize the toe by gently pulling on it and stretching it into extension.
Strengthening of muscles is key to prevent recurrence of injury and it can also help with mobility. Heel raises on the edge of a step can both strengthen the calf and stretch it at the same time with the load of your bodyweight. Hip strengthening has also been shown to help people dealing with plantar fasciitis according to Lee, et al. The hips have much bigger muscles in the glutes which can play a role in stability, so strengthening with lateral steps, squats, step ups, and a host of other exercises can help protect the plantar fascia.
Plyometrics are important to introduce if a return to running or jumping is desired. Pogo hops can be helpful to build resilience of the calf and foot muscles before more aggressive jumps are utilized. To perform the exercise, simply jump while keeping your knees relatively straight, as if you were jumping rope. Eventually you can progress the jump height and speed as you get more comfortable and your pain remains under control.
Finally, it is crucial to manage your workload. Research by Riddle, et al. revealed that working on your feet for most of the day increases your risk of plantar fasciitis. While standing in place may not seem like a lot, it can quickly add up in terms of stress. Monitoring your standing time and eventually walking and running can allow for a safe, progressive return to activity without creating more flare ups of symptoms.
As always, if you are suffering from pain, nerve symptoms (numbness, tingling, or weakness), or anything else significant, please see a healthcare provider. This blog is meant to be educational and is not a substitute for medical advice.
Hopefully you learned something about plantar fasciitis and its symptoms and treatment. If you have interest in other foot/ankle injuries, check out our ankle page. If you found this blog helpful, please share it with someone. We hope to continue to grow and help people better understand how our bodies move and work. If you want to subscribe so that you don’t miss any other posts, click the sign in button on the top right of this page. Once you have created an account, click the drop-down menu in the top right next to your name and go to your settings page. Click the subscribe button next to “Blog Subscription” and you won’t miss any future posts! If you are in the Sterling, Virginia area and would like to work with me or you have any questions, please email me at danny@eclipsewellnessnova.com or follow me on Instagram or Twitter @drdannydpt.




Comments